Impacted Wisdom Teeth (Third Molars) on the Upper East Side, Manhattan
Why Choose Dr. Min for Wisdom Tooth Care
- Columbia-trained prosthodontist coordinating evidence-based diagnosis and treatment with trusted oral surgeons.
- Award-winning precision and military-honed discipline—expect clear explanations, meticulous records, and calm guidance from consult to recovery.
- Right-time, right-case approach: remove when risks outweigh benefits; monitor when safe.
- Digital imaging (low-dose X-rays/CBCT when indicated) to evaluate roots, nerves, and sinuses before any surgery.
What Is an Impacted Wisdom Tooth?
An impacted wisdom tooth is a third molar that cannot fully erupt due to limited space or angulation. It may be:
- Soft-tissue impacted (covered by gum)
- Partial-bony impacted (partially covered by bone)
- Full-bony impacted (fully encased in bone)
Common Problems Caused by Impacted Third Molars
- Pericoronitis (gum infection) around partly erupted teeth
- Cavities & gum disease on the second molar behind the impaction
- Cysts or damage to nearby roots/bone (rare but important)
- Crowding myth: wisdom teeth aren’t a primary cause of front-tooth crowding, but they can harm the second molar if neglected.
Do All Wisdom Teeth Need Removal?
Not always. We consider: age, position, cleansability, proximity to nerves/sinus, history of infections, and risk to the second molar. Some fully erupted, easily cleaned teeth are best monitored with periodic imaging.
How We Diagnose
- Focused exam and symptom review (pain, swelling, bite changes)
- Panoramic X-ray to visualize teeth and anatomy
- CBCT 3D scan when roots are close to the inferior alveolar nerve (lower) or sinus floor (upper)
- Risk–benefit discussion (remove vs monitor; timing)
Treatment Options We Provide/Coordinate
- Observation & hygiene coaching with scheduled re-checks when low risk
- Simple extraction for erupted teeth (in-office under local anesthesia)
- Surgical extraction for impacted teeth with our oral surgery partners
- Sedation options (with surgeon): IV sedation or nitrous for comfort
- Coronectomy (surgeon-performed) in select high-risk, nerve-adjacent lower molars
- Antibiotics/pain control only when clinically indicated
The Process at a Glance
1) Consultation & Imaging
Confirm position/risks; review options, timelines, and recovery.
2) Pre-Op Planning
Insurance verification, prescriptions (if needed), and sedation instructions (NPO/escort for IV sedation with surgeon).
3) Procedure Day
Local anesthesia; surgical removal with gentle tissue handling and irrigation. Stitches placed as needed.
4) Recovery & Follow-Up
Written aftercare, check-in call, and suture removal/virtual review as indicated.
Comfort & Safety
- Profound local anesthesia with gentle technique
- Rubber bite blocks and careful lip/tongue protection
- CBCT-informed planning when anatomy is close to nerves/sinus
- Sedation by board-certified partners; sterile, single-use supplies
Recovery Timeline & Aftercare
Day 0–1
- Bite on gauze 30–45 min to control bleeding; small oozing is normal.
- Ice cheeks (20 min on/off) and keep head elevated.
- Medications: usually ibuprofen + acetaminophen; take as directed. Avoid aspirin.
- No smoking/vaping and no straws for 72 hours (dry-socket risk).
- Soft, cool foods; hydrate well.
Day 2–3
- Swelling/bruise may peak then improve. Transition to lukewarm salt-water rinses (gentle) after meals.
- Continue soft foods (yogurt, eggs, pasta, smoothies with spoon).
Day 4–7
- Gradual return to normal diet as comfortable (avoid hard, spicy, or seedy foods in the area).
- Resume light exercise after day 3–4 if no throbbing/bleeding.
Call Us Promptly If
- Bleeding that won’t stop with firm gauze pressure
- Worsening swelling after day 3, fever, foul taste/odor, or severe pain (possible dry socket)
- Persistent numbness, swallowing/breathing difficulty, or sinus fluid through the nose after upper molar removal
What to Eat (Easy Ideas)
- Day 1–2: smoothies (no straw), mashed potatoes, yogurt, applesauce, broths, scrambled eggs
- Day 3–5: soft pasta, fish, tofu, rice bowls, oatmeal
- Avoid nuts, chips, seeds, carbonated alcohol drinks, and very hot/spicy foods early on.
Cost, Insurance & Timing
- Transparent, itemized estimate based on impaction type (soft-tissue/partial-/full-bony) and number of teeth.
- Most PPO plans cover extractions; sedation coverage varies—our team verifies and files claims.
- Ideal removal age is often late teens/early 20s when roots are shorter and healing is faster, but adults benefit too with proper planning.
Frequently Asked Questions
Will I need all four removed?
Only if they’re problematic or likely to become so. We tailor the plan to
your anatomy and risk.
How long is recovery?
Typical downtime is
2–3 days for soft-tissue/partial-bony and
3–5 days for full-bony impactions; most patients resume normal routines in a week.
What is dry socket?
Loss of the protective blood clot exposing bone—causes throbbing pain day 3–5. Avoid straws/smoking; we can place soothing dressings if it occurs.
Could removal damage a nerve or the sinus?
Risk is
case-dependent. We use panoramic/CBCT imaging and, when needed, techniques like
coronectomy or surgical referral to minimize risk.
Do wisdom teeth cause crowding?
They don’t typically push front teeth forward, but they can
harm the second molar or trap plaque—another reason thoughtful monitoring/removal matters.
About Dr. Daniel Min
BA, University of Texas at Austin
DDS, University of Texas (American Esthetic Dental Association award; “Student of the Year” in clinical performance)
MS in Prosthodontics, Columbia University; former part-time clinical professor
U.S. Army veteran; current Army Reserve officer
Member: Academy of Prosthodontics; International Congress of Oral Implantologists
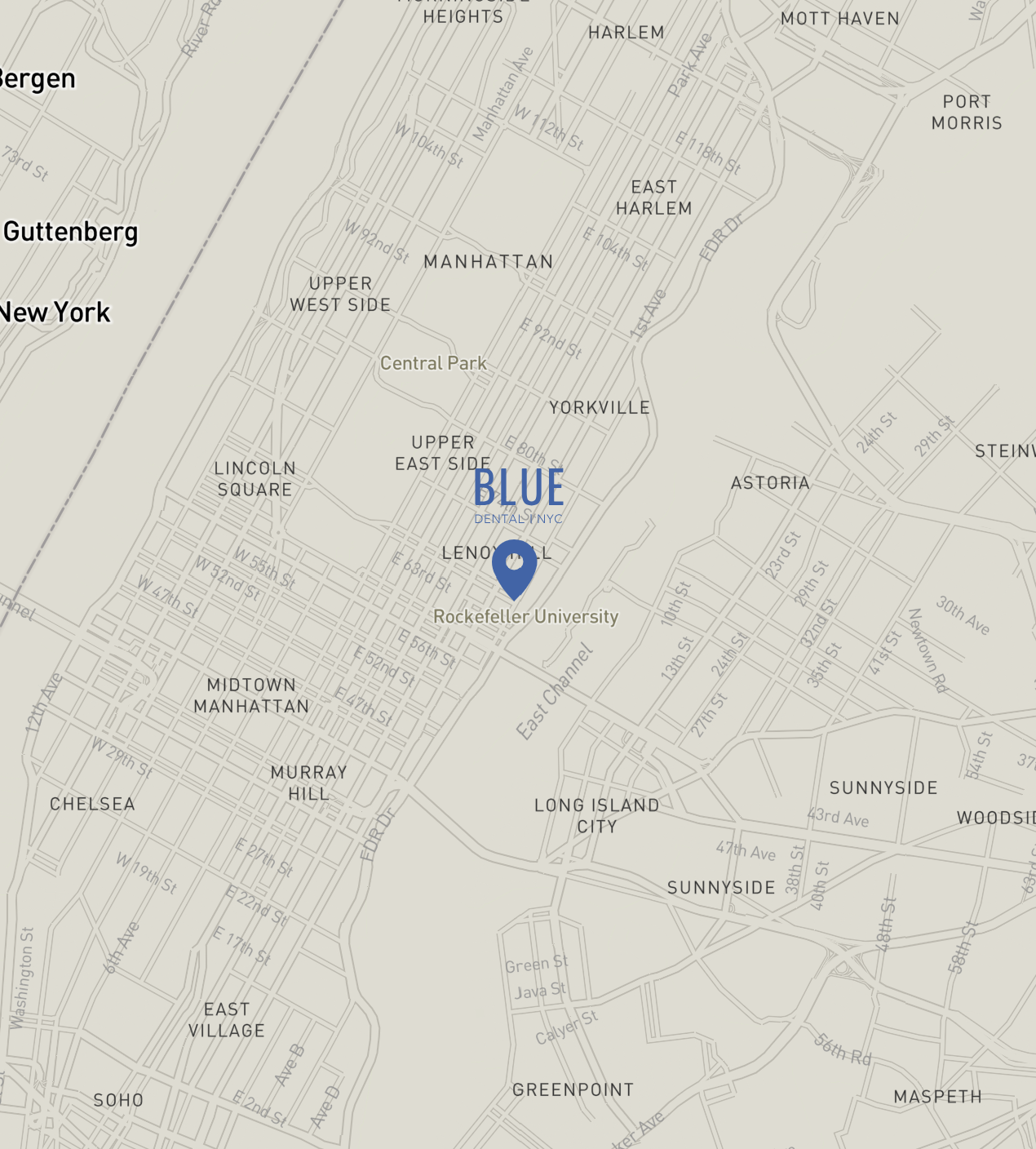
Service Area
Conveniently located on the Upper East Side and serving patients across Manhattan and the greater New York City area.
Call to Action
Wisdom tooth pain, swelling, or recurring gum flare-ups?
Book an impacted wisdom teeth evaluation with Blue Dental NYC for clear answers, imaging-based planning, and coordinated, comfortable care.